We deliver to you every day from 7:00 to 23:00
The best discounts this week
Every week you can find the best discounts here.
The Strongest Painkillers: Finding the Right Solution for Intense Pain Relief
When it comes to managing severe pain, finding the right painkiller is crucial. Whether you’re dealing with post-surgical pain, chronic conditions like arthritis, or injury-related pain, understanding your options can make all the difference. In this article, we’ll dive into the strongest painkillers, how they work, and their potential risks and benefits, so you can make an informed decision about your pain management.

What Are Strong Painkillers?
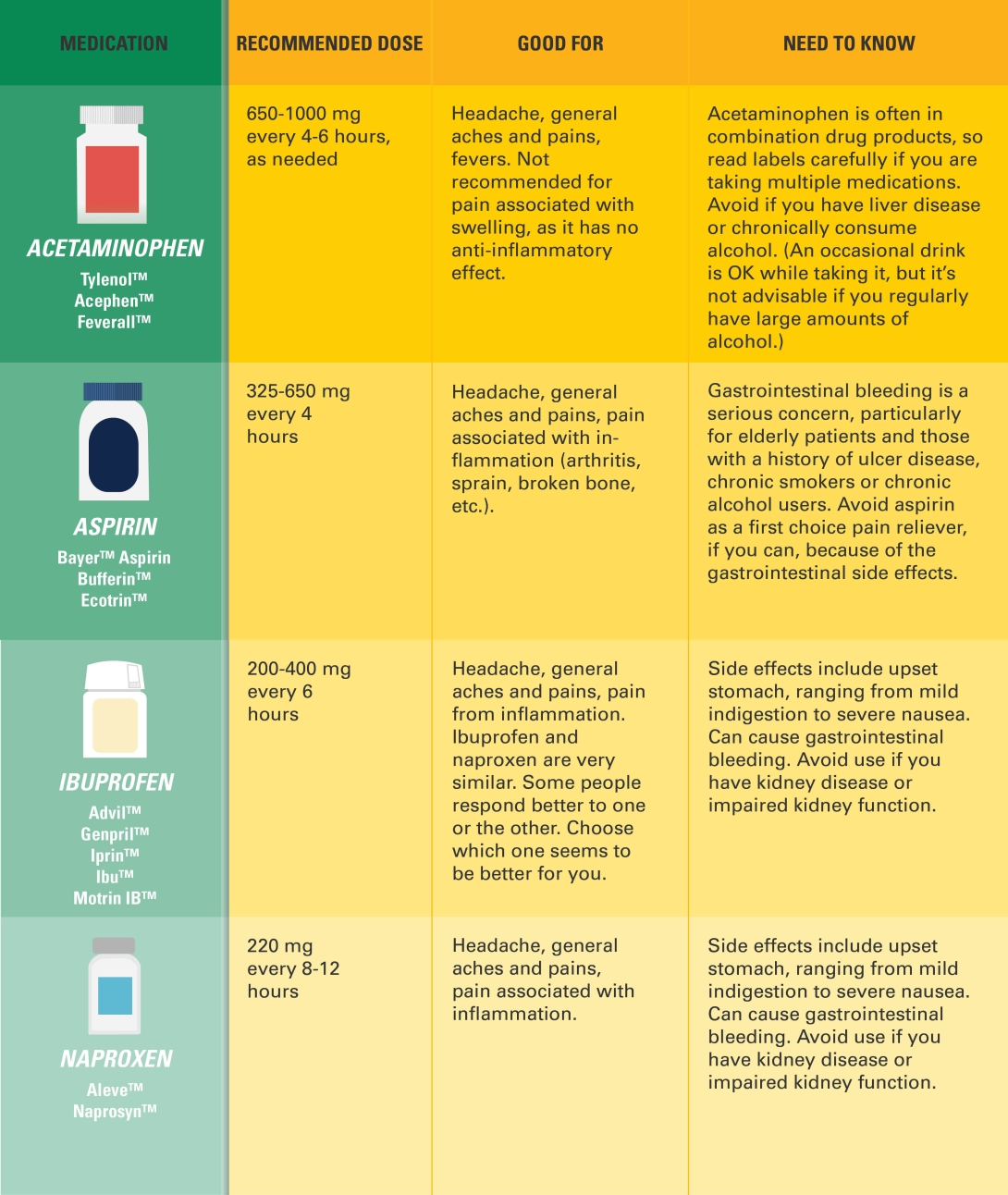
Painkillers, also known as analgesics, are medications that help alleviate pain. They work by blocking pain signals from reaching the brain or by altering the way the brain perceives pain. Stronger painkillers are typically used when mild over-the-counter (OTC) medications, like acetaminophen or ibuprofen, aren’t enough to manage the discomfort.
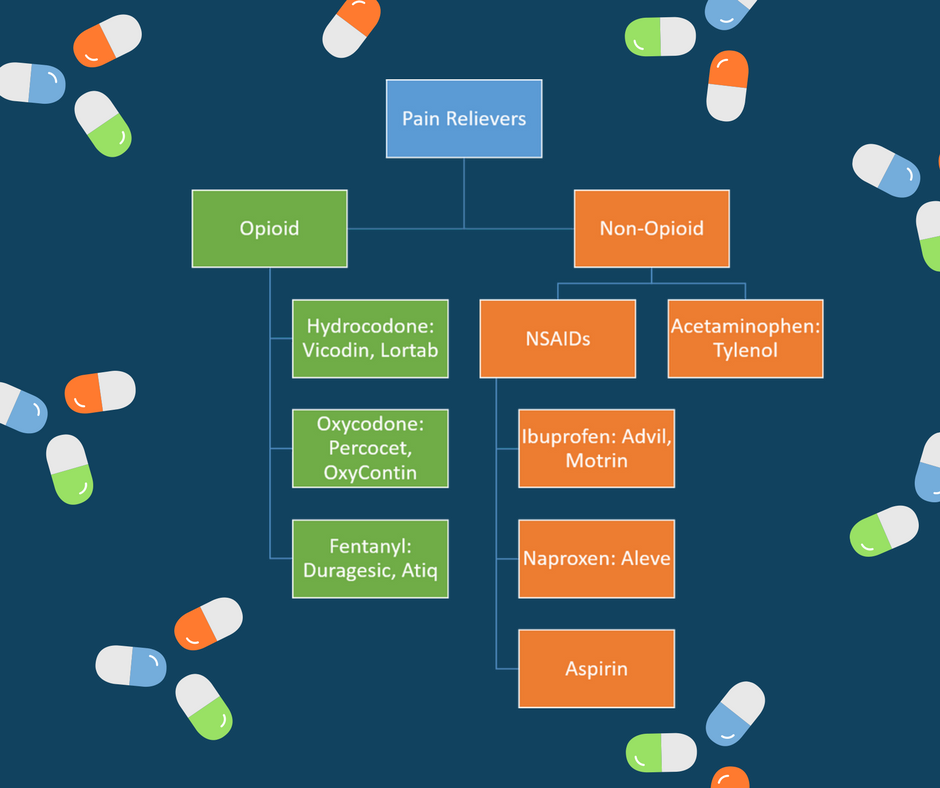
The strongest painkillers fall into two main categories: opioids and prescription-strength non-steroidal anti-inflammatory drugs (NSAIDs).
Types of Strong Painkillers
1. Opioids
Opioids are some of the most powerful painkillers available. They are used for severe pain, often following surgery or for chronic conditions like cancer.
-
How They Work: Opioids bind to opioid receptors in the brain and spinal cord to block pain signals and trigger a sense of well-being or euphoria. They can provide immediate and significant pain relief.
-
Common Opioids: Morphine, hydrocodone, oxycodone, fentanyl, and codeine.
-
Uses: Severe pain, such as post-surgical pain, cancer pain, and injury-related pain.
-
Side Effects: Opioids carry significant risks, including addiction, respiratory depression, nausea, and drowsiness. Long-term use can lead to dependence and overdose.
2. Prescription NSAIDs
Prescription-strength NSAIDs are stronger than over-the-counter versions like ibuprofen and naproxen. They are typically prescribed when inflammation and pain are present, such as in conditions like rheumatoid arthritis or osteoarthritis.
-
How They Work: NSAIDs block cyclooxygenase enzymes (COX-1 and COX-2), which are involved in producing prostaglandins—chemicals that promote inflammation, pain, and fever.
-
Common Prescription NSAIDs: Indomethacin, celecoxib, and ketorolac.
-
Uses: Chronic pain from arthritis, injuries, and muscle inflammation.
-
Side Effects: Long-term use can cause gastrointestinal bleeding, ulcers, kidney damage, and high blood pressure.
3. Corticosteroids
Corticosteroids, such as prednisone and methylprednisolone, are often prescribed for inflammatory conditions. Though not classified as traditional painkillers, they are used to reduce swelling and inflammation in conditions like arthritis, which can provide pain relief.
-
How They Work: These medications suppress the immune system and reduce inflammation, providing relief from pain caused by swelling or irritation of tissues.
-
Uses: Arthritis, lupus, allergic reactions, and respiratory conditions like asthma.
-
Side Effects: Long-term use can lead to osteoporosis, weight gain, and increased infection risk.
4. Ketamine
Ketamine is a dissociative anesthetic that has gained attention as a strong pain reliever, particularly in the treatment of chronic pain and neuropathic pain.
-
How It Works: Ketamine works by blocking NMDA receptors in the brain, which are involved in pain transmission. It is particularly effective for pain that doesn’t respond well to traditional analgesics.
-
Uses: Severe chronic pain, neuropathic pain, and post-surgical pain.
-
Side Effects: Possible side effects include hallucinations, nausea, and high blood pressure.
5. Topical Medications
For localized pain, topical medications can be highly effective in delivering strong pain relief without affecting the rest of the body.
-
How They Work: Topical treatments, such as lidocaine patches or capsaicin cream, are applied directly to the skin. They work by numbing the pain receptors or reducing inflammation in the targeted area.
-
Uses: Localized muscle pain, joint pain, and nerve pain.
-
Side Effects: Rare, but may include skin irritation or allergic reactions.
How to Choose the Right Strong Painkiller
Choosing the strongest painkiller for your needs depends on the type and intensity of your pain. For example, opioids may be appropriate for acute pain following surgery, but their high risk of addiction and side effects means they should only be used under strict medical supervision.
For chronic inflammatory conditions, prescription-strength NSAIDs or corticosteroids might offer better long-term relief. Topical treatments are ideal for localized pain and provide fewer systemic side effects.
If you’re unsure, consult your healthcare provider to determine the most suitable medication based on your individual circumstances.
Risks and Side Effects of Strong Painkillers
While strong painkillers can offer effective relief, they come with potential risks. Here’s a breakdown of some of the most common side effects:
-
Opioids: Addiction, respiratory depression, drowsiness, and nausea.
-
NSAIDs: Gastrointestinal issues like ulcers, kidney damage, and increased bleeding risk.
-
Corticosteroids: Weight gain, high blood pressure, and osteoporosis.
-
Ketamine: Hallucinations, increased blood pressure, and nausea.

Managing Pain Effectively: Combining Medications
In some cases, a combination of pain relief strategies may be the most effective solution. For example, a doctor may recommend using NSAIDs for inflammation and adding an opioid for severe pain after surgery. Topical treatments may also be used alongside oral medications for localized pain.
However, combining different medications requires careful monitoring to avoid dangerous interactions and side effects. Always follow your healthcare provider’s instructions and avoid mixing strong painkillers without professional guidance.
When to Seek Medical Advice
If you experience any of the following, it’s important to consult a healthcare provider immediately:
-
Severe side effects like dizziness, confusion, or difficulty breathing.
-
Pain that persists or worsens despite medication.
-
Signs of addiction or dependence on pain medications.
-
New symptoms, such as stomach pain or bloody stools, while taking NSAIDs or opioids.
FAQs About Strong Painkillers
1. What is the strongest painkiller available?
Opioids, such as fentanyl, are considered the strongest painkillers for severe pain. However, due to their risk of addiction, they are prescribed with caution.
2. Can I take a strong painkiller for long-term pain management?
Long-term use of strong painkillers, especially opioids, is generally not recommended due to the risk of addiction and other side effects. For chronic pain, your doctor may recommend alternative treatments, such as physical therapy or non-opioid medications.
3. Are there any natural alternatives to strong painkillers?
Yes, natural remedies such as turmeric (curcumin), CBD oil, and acupuncture have been shown to provide mild pain relief. However, they are typically not as effective for severe pain compared to prescription medications.
4. How can I avoid the side effects of strong painkillers?
To minimize side effects, follow your doctor’s instructions carefully, take the medication at the lowest effective dose, and avoid combining painkillers with alcohol or other drugs. Regular check-ups with your healthcare provider can also help monitor for adverse effects.
Conclusion
Choosing the strongest painkiller for your situation is essential for effective pain management. While opioids are the strongest option for acute, severe pain, they come with significant risks. Prescription-strength NSAIDs, corticosteroids, and topical treatments are valuable alternatives for various pain conditions. Always work closely with your healthcare provider to find the best approach for your pain relief while minimizing risks.
By understanding the available options and their potential risks and benefits, you can make more informed decisions and manage your pain safely and effectively.