We deliver to you every day from 7:00 to 23:00
The best discounts this week
Every week you can find the best discounts here.
How Do Painkillers Affect the Kidneys?
Painkillers are commonly used to relieve discomfort and improve quality of life. However, while effective for pain management, these medications can have significant effects on the kidneys, especially when taken improperly or over long periods. In this article, we will explore how painkillers affect the kidneys, the risks involved, and how to use them safely to protect your health.
Types of Painkillers and Their Effects on the Kidneys
Painkillers, also known as analgesics, come in several forms, each with its potential impact on kidney function. The most commonly used types are nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen (Tylenol), and opioids. Here’s a breakdown of how each type affects kidney health:
1. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs, such as ibuprofen, naproxen, and aspirin, are commonly used to reduce inflammation, pain, and fever. However, these drugs can harm the kidneys when used for extended periods or in high doses.
-
Impact on Kidneys: NSAIDs block the production of certain chemicals (prostaglandins) that help maintain blood flow to the kidneys. This can lead to kidney damage, particularly in individuals with existing kidney conditions or those who are dehydrated.
-
Risk Factors: People with high blood pressure, diabetes, or a history of kidney disease are at higher risk of kidney damage when taking NSAIDs.
For a deeper understanding of the risks of painkillers, you can explore more in this article on painkiller safety.
2. Acetaminophen (Tylenol)
Acetaminophen is one of the most commonly used painkillers, found in many over-the-counter medications. While it’s generally considered safe for occasional use, long-term or excessive consumption can cause harm.
-
Impact on Kidneys: Acetaminophen is processed by the liver, but overuse can also affect the kidneys, especially in high doses. Prolonged use can lead to acute kidney injury, particularly when combined with other medications or in individuals with pre-existing kidney conditions.
-
Risk Factors: The risk is higher in individuals who regularly consume alcohol or have liver disease.
How Painkillers Contribute to Kidney Damage
Painkillers, when taken improperly or for extended periods, can cause both acute and chronic kidney problems. Let’s dive into the different ways painkillers contribute to kidney damage:
1. Acute Kidney Injury (AKI)
One of the most serious risks of taking painkillers is acute kidney injury (AKI). AKI occurs when the kidneys suddenly lose their ability to filter waste and maintain fluid balance. This can be caused by:
-
Dehydration: NSAIDs can worsen dehydration, which reduces blood flow to the kidneys, leading to kidney damage.
-
Overdose or Long-Term Use: Taking large amounts of painkillers or using them over long periods can overwhelm the kidneys, leading to acute kidney injury.
2. Chronic Kidney Disease (CKD)
Long-term use of painkillers can lead to chronic kidney disease (CKD). This condition develops gradually and can lead to kidney failure if not managed properly. People who use painkillers frequently, especially NSAIDs, are at a higher risk of developing CKD due to:
-
Reduced Blood Flow to the Kidneys: NSAIDs reduce the production of prostaglandins, which help maintain blood flow to the kidneys. This can cause kidney tissues to suffer from a lack of oxygen and nutrients over time.
-
Inflammation and Scarring: Overuse of painkillers can lead to long-term inflammation, causing scarring and damage to kidney tissues.
Risks for Vulnerable Populations
Certain groups of people are more susceptible to kidney damage from painkillers. It’s important to be aware of these risks:
1. Older Adults
As people age, their kidneys naturally lose some of their function. Older adults are more likely to have other underlying health conditions, such as high blood pressure or diabetes, which can compound the risks of painkiller use.
-
Higher Sensitivity: Older individuals may be more sensitive to the effects of painkillers, even at lower doses.
-
Cumulative Damage: Long-term use of painkillers can lead to a cumulative effect, increasing the risk of both acute and chronic kidney damage.
2. People with Pre-existing Kidney Conditions
Individuals with a history of kidney disease, high blood pressure, or diabetes should be especially cautious when taking painkillers. These conditions already put extra strain on the kidneys, and painkillers can exacerbate the damage.
-
Pre-existing Damage: If the kidneys are already damaged, taking NSAIDs or acetaminophen can accelerate the decline in kidney function.
3. Dehydrated Individuals
People who are dehydrated or have conditions that lead to dehydration, such as diarrhea or vomiting, should avoid taking NSAIDs. Dehydration reduces the blood flow to the kidneys, which can significantly increase the risk of kidney damage.

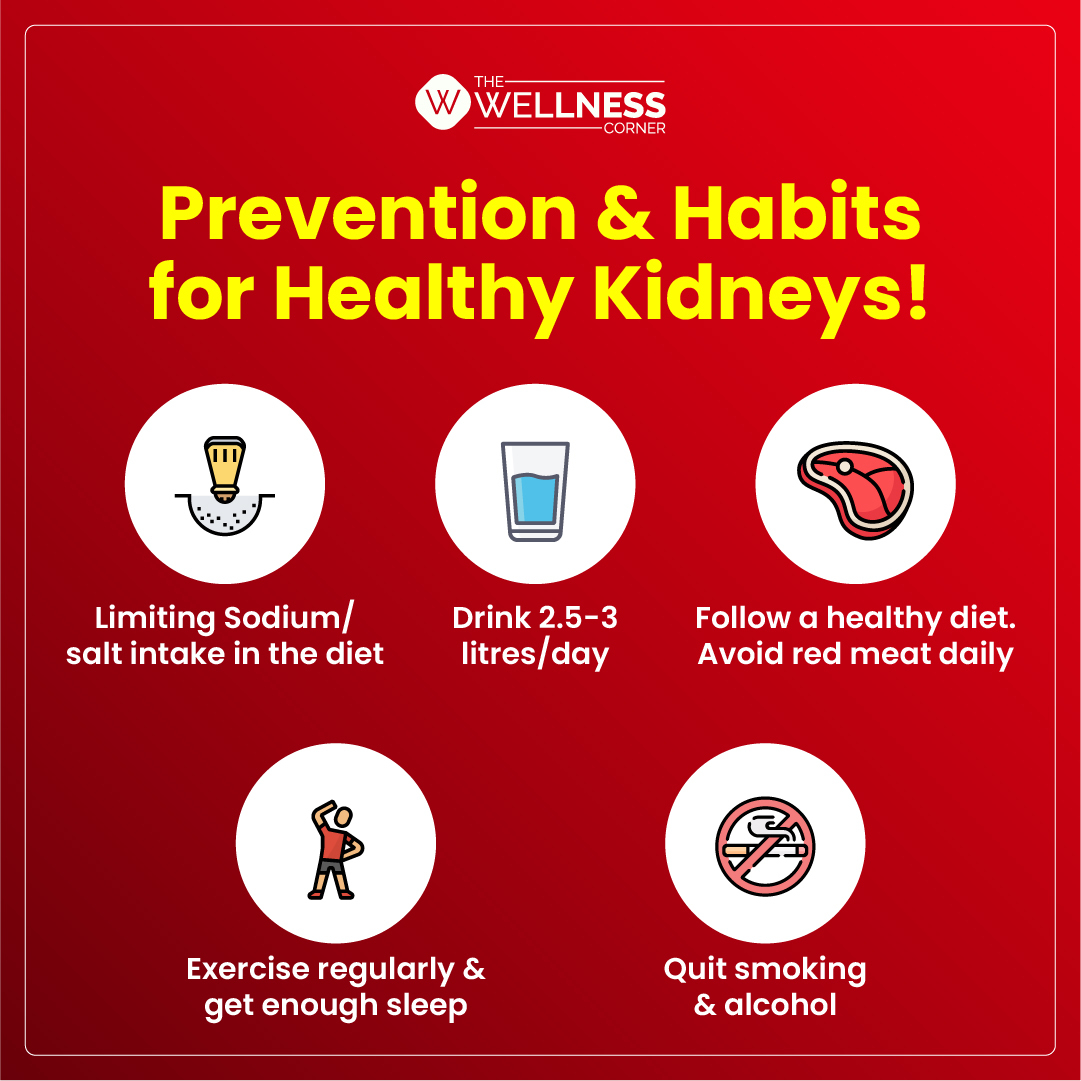
Safe Use of Painkillers to Protect Kidney Health
While painkillers can be harmful to the kidneys, there are steps you can take to minimize the risks. Here are some tips for using painkillers safely:
1. Use the Lowest Effective Dose
Always take the lowest effective dose of painkillers, and avoid using them for long periods unless directed by a doctor. This reduces the likelihood of kidney damage while still managing pain effectively.
2. Stay Hydrated
Ensuring you stay properly hydrated is crucial, especially when using NSAIDs. Drink plenty of fluids throughout the day to help maintain healthy blood flow to your kidneys and prevent dehydration.
3. Consult a Doctor Before Long-Term Use
If you require pain relief on a long-term basis, it’s important to consult a doctor about the best options for managing pain without harming your kidneys. Your doctor may recommend alternative treatments or medications that are safer for your kidneys.
4. Regular Monitoring of Kidney Function
If you must take painkillers regularly, it’s important to have your kidney function monitored periodically. This includes blood tests to check for any signs of kidney damage, especially if you have risk factors like diabetes or high blood pressure.
When to Seek Medical Advice
If you experience any of the following symptoms while taking painkillers, it’s essential to seek medical advice:
-
Swelling in the legs, ankles, or feet, which could indicate kidney problems.
-
Fatigue or weakness, which may be a sign of kidney dysfunction.
-
Changes in urine output, such as dark urine or reduced urination.
-
Nausea, vomiting, or confusion, which could be signs of kidney damage.
Frequently Asked Questions
1. Can painkillers cause kidney failure?
Yes, prolonged or excessive use of painkillers, particularly NSAIDs, can lead to kidney failure over time, especially if combined with other risk factors like dehydration, pre-existing kidney disease, or high blood pressure.
2. Is acetaminophen safer than NSAIDs for the kidneys?
Acetaminophen is generally considered less harmful to the kidneys than NSAIDs when used in recommended doses. However, excessive use of acetaminophen can still cause liver and kidney damage, especially in those with pre-existing liver conditions.
3. How can I protect my kidneys while taking painkillers?
To protect your kidneys, use the lowest effective dose of painkillers, stay hydrated, and avoid long-term use. If you have pre-existing kidney conditions or other risk factors, consult your doctor for alternative pain management options.
Conclusion
Painkillers, when used correctly, can provide significant relief from pain. However, improper use, especially of NSAIDs and acetaminophen, can cause serious kidney damage. To protect your kidney health, always follow recommended dosages, stay hydrated, and consult your doctor before using painkillers for extended periods. By taking these precautions, you can manage pain while minimizing the risk of kidney damage.
For more information on safe pain management and health tips, visit DUYTHIN.DIGITAL, where we specialize in providing advanced automation tools for platforms like Facebook, Zalo, and more.